Paper: Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore
Wong, J., Goh, Q. Y., Tan, Z., Lie, S. A., Tay, Y. C., Ng, S. Y., & Soh, C. R. (2020). Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Canadian Journal of Anesthesia/Journal canadien d'anesthésie, 1-14.
Important quotation:


Important quotation:
Abstract
The coronavirus disease 2019 (COVID-19) outbreak has been designated a public health emergency of international concern. To prepare for a pandemic, hospitals need a strategy to manage their space, staff, and supplies so that optimum care is provided to patients. In addition, infection prevention measures need to be implemented to reduce in-hospital transmission. In the operating room, these preparations involve multiple stakeholders and can present a significant challenge. Here, we describe the outbreak response measures of the anesthetic department staffing the largest (1,700-bed) academic tertiary level acute care hospital in Singapore (Singapore General Hospital) and a smaller regional hospital (Sengkang General Hospital). These include engineering controls such as identification and preparation of an isolation operating room, administrative measures such as modification of workflow and processes, introduction of personal protective equipment for staff, and formulation of clinical guidelines for anesthetic management. Simulation was valuable in evaluating the feasibility of new operating room set-ups or workflow. We also discuss how the hierarchy of controls can be used as a framework to plan the necessary measures during each phase of a pandemic, and review the evidence for the measures taken. These containment measures are necessary to optimize the quality of care provided to COVID-19 patients and to reduce the risk of viral transmission to other patients or healthcare workers.
Important quotation:
1. Communications and staff support
In the early phase of the outbreak, the situation was rapidly evolving so case definitions and hospital guidelines were modified frequently. Communication channels including a COVID-19 website were set up and daily email updates were sent to all staff. Staff used social media, such as Workplace from Facebook and encrypted instant messaging, to approach senior management with ideas or concerns.13
Resources, including reading material and a helpline, were set up in the hospital to help staff cope with COVID-19-related anxiety and burnout.13
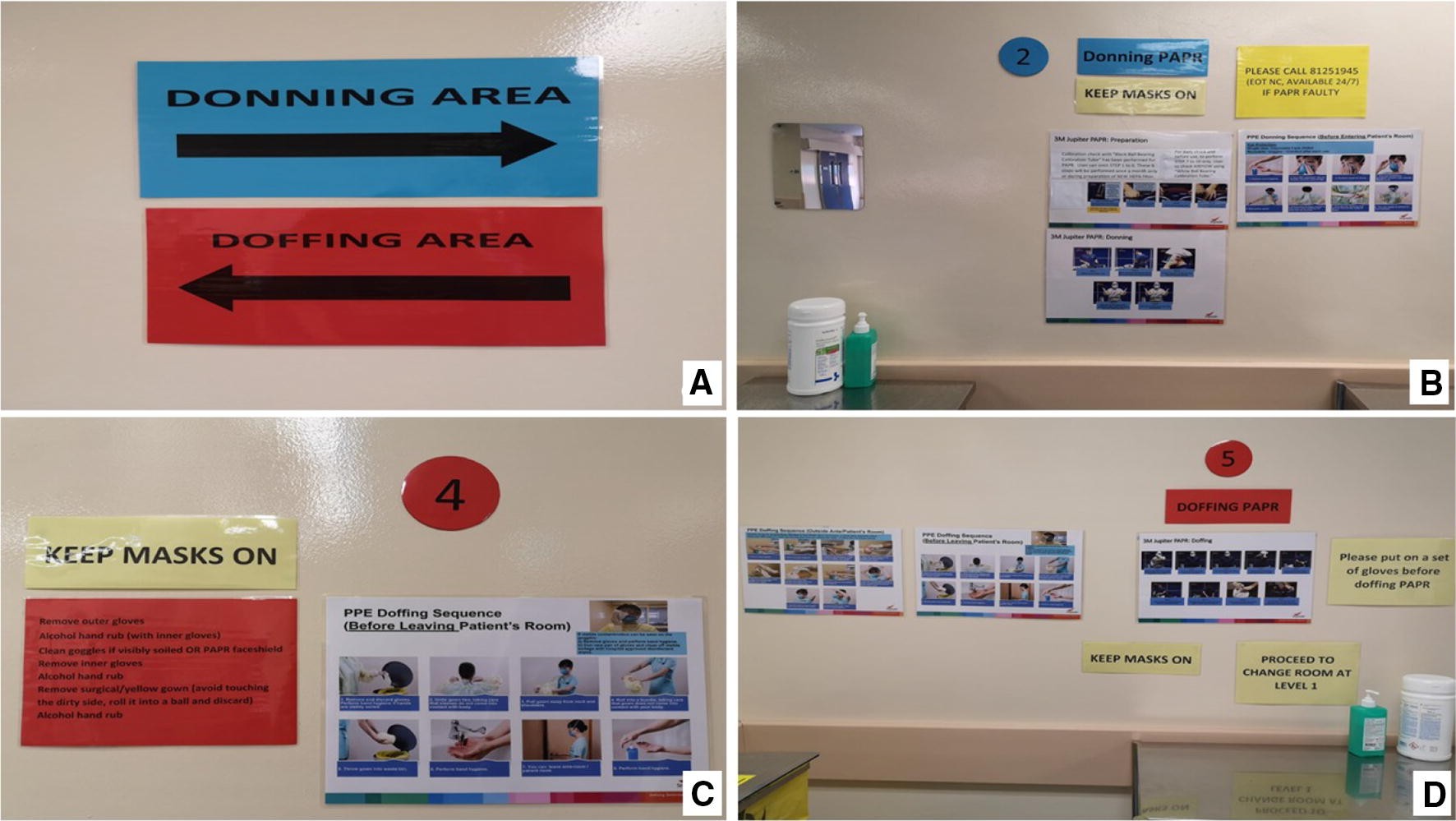
2. Personal Protective Equipment and Doffing areas
Personal protective equipment donning and doffing areas. Steps are colour-coded (A: blue for clean and red for contaminated) and marked in numerical sequence at designated areas just outside the OR, with posters to guide staff on the process. Step 1: Put on N95. Step 2: Donning PAPR (B). Step 3: Enter OR through scrub room. Step 4: Clean external surface of the PAPR face shield (C), remove surgical gown and outer gloves. Step 5: Doffing PAPR (D). OR = operating room; PAPR = powered air-purifying respirator.
3. The importance of the contaiment measures
These containment measures- 1) engineering controls (such as identification and preparation of an isolation operating room, administrative measures such as modification of workflow and processes, introduction of personal protective equipment for staff, and formulation of clinical guidelines for anaesthetic management); 2. simulation; 3) hierarchy of control (a framework to plan & review the evidence)-are necessary to optimize the quality of care provided to COVID-19 patients and to reduce the risk of viral transmission to other patients or healthcare workers.
4. Management of patients, visitors, and staff
a. All patients presenting to the hospital were screened using a standard questionnaire.
b. Patients who fulfilled the criteria for suspected SARS-CoV-2 infection were isolated, referred to an infectious diseases specialist, and tested for the virus.
c. Elective surgery was postponed if the patient had travelled to affected areas. Visitor numbers were also restricted.28
d. Staff were asked to refrain from unnecessary travel to certain destinations as advised by the Singapore Ministry of Health.29
e. Staff returning from these destinations were required to take a 14-day leave of absence. We also separated staff caring for COVID-19 patients and those caring for other patients to reduce the risk of in-hospital transmission.
f. Staff who had cared for COVID-19 patients continued with usual clinical work with a surgical mask on and monitored themselves for fever and respiratory symptoms.
g. If inadequate personal protective equipment (PPE) was worn at the time of close contact, the staff member was taken off duty while an infectious diseases team assessed the risk of transmission and planned subsequent management.
h. Temperatures of all staff were taken twice daily using hospital-issued oral digital thermometers, and entered into electronic records monitored by administrative personnel.
h. Web-based forms were created to facilitate ease of entry using personal smartphones. Staff members who developed a fever or respiratory symptoms were screened at the staff clinic.
5. Infection prevention when caring for the COVID-19 patient
The minimum standard of PPE for any staff caring for a patient with confirmed/suspected COVID-19 infection is a fitted, NIOSH-certified N95 respirator, eye protection (either goggles or full-face shield), cap, gown, and gloves.5 Double gloves may be considered and the outer pair should be changed when contaminated.31 As transmission remains possible despite N95 protection,32 staff participating in aerosol-generating procedures can wear a PAPR
Figure: Staff in powered air-purifying respirator (PAPR) during an aerosol-generating procedure

High-touch equipment within the operating room are wrapped with plastic sheets to facilitate decontamination. A) Anesthesia workstation. B) Back of anesthesia workstation. C) Exposed surfaces wrapped with plastic. D) Laptop for nursing documentation

Conclusions
Preparation for a pandemic involves considering the different levels in the hierarchy of controls as well as the different phases of the pandemic. In the OR setting, these measures include the modification of infrastructure and processes, management of staff and patients, infection prevention strategies, and clinical recommendations. The OR is a complex environment with multiple stakeholders including anesthesiologists, surgeons, nurses, OR attendants, and technicians; it can be a challenge to align the interests and concerns of all parties. Nevertheless, we believe that these containment measures are necessary to optimize the quality of care provided to COVID-19 patients and to reduce the risk of viral transmission to other patients or healthcare workers.


Comments
Post a Comment