PAPER: nderstanding women's uptake and adherence in Option B+ for prevention of mother-to-child HIV transmission in Papua, Indonesia: A qualitative study.
Understanding women’s uptake and adherence in Option B+ for prevention
of mother-to-child HIV transmission in Papua, Indonesia: A qualitative study
Reference
Lumbantoruan, C., Kermode,
M., Giyai, A., Ang, A., & Kelaher, M. (2018). Understanding women's uptake
and adherence in Option B+ for prevention of mother-to-child HIV transmission
in Papua, Indonesia: A qualitative study. PloS one, 13(6),
e0198329.
Christina Lumbantoruan1,2*,
Michelle Kermode2,
Aloisius Giyai3,
Agnes Ang3,
Margaret Kelaher1
1 Centre for Health
Policy, University of Melbourne, Melbourne, Victoria, Australia, 2 Nossal
Institute for Global Health, University of Melbourne, Melbourne, Victoria,
Australia, 3 Provincial Health Office, Papua Provincial Health Office,
Jayapura, Papua, Indonesia
MY CONCLUSION:
Methodology
|
Result 1
|
Result 2
|
Result 3
|
Summary
|
In-depth Interview
20 women living with HIV (10 women who were non-adherent,
10 women who were 100% adherence)
20 PMTCT workers at two main referral hospitals for PMTCT
in Papua
Pregnant and postpartum
HIV-positive women with live birth who attended the ANC at Jayapura Hospital
and Abepura Hospital, as well as health workers who provided PMTCT services
at both health facilities.
|
Supportive factors of PMTCT uptake and adherence:
*Good quality post-test HIV counselling
*Belief in the efficacy of ARV
*a partner who did not prevent women from seeking PMTCT
care; sero discordant and HIV positive partners were more reported to be more
supportive than partners who refused to get tested
*good relationship with health workers
*No. discrimination in health setting:No. excessive use of
precautions, including masks, and gloves
|
Key barriers for PMTCT participation:
*doubts of ARV efficacy, particularly for asymptomatic
women
*unsupportive partners
*Women’s concerns about community stgma and discrimination
*long-waiting list in hospital
|
Strategies to enhance women’s engagement to pmtct services: counselling
women with doubts regarding arv efficacy early program: enhancment of support
for women in need; a continuous campaigns; availability of adequate human
resources; reduction of long waiting times, and increased privacy during
return visits
|
Concern of long-term
adherence for long-term of accessing PMTCT service
Option B+ as current national
policy for pregnant women in Papua has improved detection and enrolment of
HIV-positive women, health facilities need to address various existing and
potential issues to ensure long-term adherence of women beyond the current
PMTCT program, including during pregnancy, childbirth and breastfeeding.
|
Abstract
Background
Despite a more proactive
approach to reducing new HIV infections in infants through lifelong treatment
(Option B+ policy) for infected pregnant women, prevention of mother-to-child
transmission of HIV (PMTCT) has not been fully effective in Papua, Indonesia.
Mother-to- child transmission (MTCT) is the second greatest risk factor for HIV
infection in the commu- nity, and an elimination target of <1% MTCT has not
yet been achieved. The purpose of this study was to improve understanding of
the implementation of Option B+ for PMTCT in Papua through investigation of
facilitators and barriers to women’s uptake and adherence to antiretroviral
therapy (ART) in the program. This information is vital for improving program
outcomes and success of program scale up in similar settings in Papua.
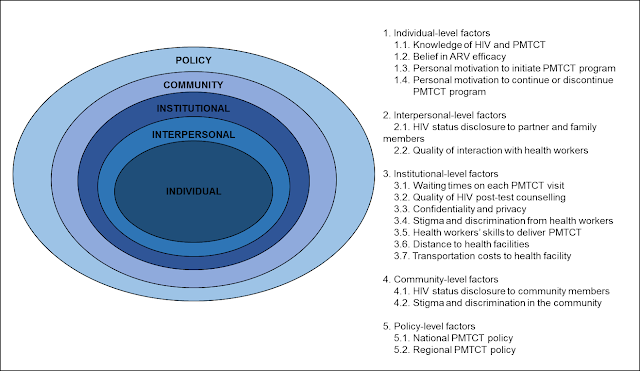
Methods
In-depth interviews were
conducted with 20 women and 20 PMTCT health workers at
two main referral hospitals for PMTCT in Papua. Development of interview guides
was informed by the socio-ecological framework.
Qualitative data were managed with NVivo11 software and themes were analysed
using template analysis. Factors influencing women’s uptake and adherence in
Option B+ for PMTCT were identified through final analysis of key themes.
Results
Factors that motivated
PMTCT uptake and adherence were good quality post-test HIV counselling, belief
in the efficacy of antiretroviral (ARV) attained through personal or peer
experiences, and a partner who did not prevent women from seeking PMTCT care.
Key barriers for PMTCT participation included doubts about ARV efficacy,
particularly for asymptomatic women, unsupportive partners who actively
prevented women from seeking treatment, and women’s concerns about community
stigma and discrimination.
Conclusions
Results suggest that PMTCT
program success is determined by facilitators and barriers from across the
spectrum of the socio-ecological model. While roll out of Option B+ as current
national policy for pregnant women in Papua has improved detection and
enrolment of HIV-positive women, health facilities need to address various
existing and potential issues to ensure long-term adherence of women beyond the
current PMTCT program, including during pregnancy, childbirth and
breastfeeding.
IMPORTANT QUOTATION
In 2012, the World Health Organization
(WHO) recommended Option B+ as a novel approach to eliminate mother-to-child
transmission (MTCT) of HIV [1]
This approach requires
routine HIV testing for all pregnant women and lifelong antiretroviral therapy
(ART) for positive cases irrespective of HIV clinical status or CD4 count [2].
Based on WHO criteria,
elimination of mother-to-child transmission (EMTCT) of HIV is achieved when
there is less than 2% MTCT in non-breastfeeding populations or less than 5% in
breastfeeding popula- tions, and if per 100,000 live births there are no more
than 50 new pediatric infections [3].
1.
World Health Organisation. Programmatic
update: Use of antiretroviral drugs for treating pregnant women and preventing
HIV infection in infants. 2012. Available from: http://www.who.int/hiv/pub/mtct/
programmatic_update2012/en/
2.
World Health Organization. Consolidated
guidelines on the use of antiretroviral drugs for treating and preventing HIV
infection: Recommendations for a public health approach. Geneva: World Health
Orga- nization. 2013.
3.
World Health Organisation. Global
guidance on criteria and processes for validation: Elimination of
mother-to-child transmission of HIV and syphilis. 2nd edition. WHO. 2014.
Available from: http://apps.
who.int/iris/bitstream/handle/10665/259517/9789241513272-eng.pdf;jsessionid=
0EB32F7E22EC7CA9EF12029AE8170794?sequence=1
Prior to Option B+, PMTCT
performance in Indonesia was suboptimal with 86 new HIV infections in 1,145
(7.5%) live births among HIV-positive women who received the interven- tion [9]. During this period, PMTCT implementation was
limited because of stigma and dis- crimination, long distances to health
facilities, and long waiting times [10–12].
4.
Kementerian Kesehatan Republik Indonesia.
Rencana aksi nasional pencegahan penularan HIV dari ibu ke anak (PPIA)
Indonesia 2013–2017. 2013. Available from: http://www.kebijakanaidsindonesia.
net/jdownloads/Publikasi%20Publication/rencana_aksi_nasional_pencegahan_penularan_hiv_dari_
ibu_ke_anak_ppia_-_2013_2017.pdf
5.
Hardon AP, Oosterhoff P, Imelda JD, Anh
NT, Hidayana I. Preventing mother-to-child transmission of HIV in Vietnam and
Indonesia: Diverging care dynamics. Social Science & Medicine. 2009; 69(6):
838– 845.
6. Oktavia M, Alban A, Zwanikken PAC. A qualitative study on HIV
positive women experience in PMTCT program in Indonesia. Retrovirology. 2012;
9. Available from: https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC3360250/pdf/1742-4690-9-S1-P119.pdf
7.
Trisnawati LM,
Thabrany H. The role of health system to support PMTCT program implementation
in Jayawijaya regency. Indonesian Health Policy and Administration. 2015; 1(1):
8. Available from: http://
journal.fkm.ui.ac.id/ihpa/article/view/1729/575
Data Analysis
The research team followed
eight steps for conducting template analysis:
Step 1. Development of a
priori themes based on literature related to the PMTCT program in Indonesia
and other low and middle income countries, as shown in Fig
1.
Step 2. Data familiarisation
by reading interview transcripts.
Step 3. Preliminary data
coding by highlighting parts of transcripts relevant to a priori themes
and new information relevant to research questions.
Step 4. Refinement of a
priori themes to integrate new emerging themes.
Step 5. Organisation of
themes into groups and establishment of hierarchical and lateral rela-
tionships between groups.
Step 6. Development of an
initial coding template after coding five interviews that contained the
greatest variation in responses.
Step 7. Application of the
initial coding template, and revision after coding of another five interviews.
Step 8. Finalisation of
the coding template and its application on the full data set.
RECRUITMENT: IN
HOSPITAL SETTING
Women
who agreed to participate were asked about their time and location preference
for interviews. All women preferred to be interviewed on the same day at the
hospital while waiting for their appointment, other than one woman who
requested to return for an interview the following day. Length of interviews
ranged from 15 to 45 minutes with an average of 29 minutes, excluding
icebreaking conversation that took around 5 minutes per interview.
Health
worker participants were individually approached by CL and were informed about
the voluntary nature of the study. All health workers (20/20) participated
voluntarily in inter- views. As preferred by health workers, interviews were
conducted at the hospitals after working hours or during less busy hours.
Duration of interviews with health workers was between 16 and 60 minutes with
an average of 38 minutes.
Result
Participant characteristic
Data from 40 interviews,
20 HIV-positive women (10 women who were non-adherent, 10 women who were 100%
adherent) and 20 health workers (health workers providing PMTCT service at both
hospitals for at least one year), were analysed.
Stigma and
discrimination at health facility: Discrimination was not observed
during field observations at both health facilities. There was no excessive
use of precautions, including masks and gloves, in executing routine tasks or
when meeting HIV+ women. Women partici- pants also claimed they were not
treated differently (20/20) after HIV diagnosis. No participant reported
discontinuing treatment due to discrimination at the health facilities. [pp 10]
Interpersonal-level
factors. HIV status disclosure and partner support: The majority of women
in this study (16/20) had disclosed their HIV status to their partners
and requested they get tested for HIV. Sero discordant and HIV positive
partners were reported to be more supportive than partners who refused to get
tested. The latter could be mentally or physically abusive, and prevented
women from adhering to treatment. The presence of domestic violence (3/10)
before and/or after HIV status disclosure became a main reason for PMTCT
non-adherence reported by women. [9]
Institutional-level
factors. Health workers explained the increasing number of patients they
managed at CST clinics because HIV+ pregnant women no longer stopped ART after
childbirth/breastfeeding as occurred pre- Option B+. They explained major infrastructure
and human resources changes were less likely to occur in the short-term, so
the PMTCT program was adjusted to meet available resources. Consequently, there
was a reduction in quality of care, such as long wait
times and lack of privacy, but women and health workers rarely identified
these as barriers to PMTCT uptake and adherence. Frequently mentioned
facilitators of program adherence were respect for
confidentiality and stigma-free care from health workers. [9]
Factors motivating uptake
and continuation in the program were a constellation of individual,
interpersonal, institutional, and policy factors. Factors associated with
increased uptake and adherence included good quality post-test HIV counselling,
belief in the efficacy of ARVs to prevent transmission
and improve health, confidentiality of HIV status, absence of stigma and
discrimination at health facilities, positive women-health worker
relationships, and free HIV services [25–32].
PERSONAL BELIEF OF
EFFICACY IN ARV, EVEN WITHOUT ACTIVE ENCOURAGEMENT FROM THEIR PARTNERS
PARTNER’S SUPPORT,
PARTICULALRY FINANSIAL SUPPORT IS STILL IMPORTANT
The women in our study
did not necessarily require a partner who actively supported their
treatment in order to remain in the program, unlike findings in other studies [23, 25, 37, 38]. A majority
of women continued their treatment due to personal
belief in ARV efficacy even without active encouragement from their partner.
However, consistent with findings of other studies, partner
support is important to retain women who are financially dependent on the
partner [25, 26,
37, 39, 40].
GOOD RELATIONSHIP WITH
HEALTH WORKERS
Women-health worker
relationships: The relationship between health workers and women seemed to
be satisfactory as all women (20/20) described health workers as either friendly
or kind, while health workers felt ‘kasihan’, or sympathy, for women and
their children. A minority of women (2/20) mentioned health workers becoming
angry with them when they missed their doses, but they believed it was ‘a sign
of caring’, rather than dislike. One woman, however, preferred health workers
explaining things without being angry. [11]
SEEKING HEALTH SERVICES
OUTSIDE THEIR NEIGHBOURHOOD: AVOID OF COMMUNITY STIGMA
Stigma and
discrimination in the community: Perceived stigma and consequent discrimination
in the community was seen by women as an important barrier to continued
participation in the PMTCT program. Hence, a large proportion of women (16/20)
sought treatment at a health facility outside of their neighborhood to avoid
detection of HIV diagnosis by family members or friends. For this group, this
meant travelling between 45 and 60 minutes using public transportation (n = 7)
or continuing PMTCT treat- ment at referral hospitals instead of returning to
nearby satellite PHCs (n = 9). Of 10 women who were adherent to PMTCT
treatment, only one woman lived less than 30 minutes from the health facility.
[11
STRATEGIES TO ENHANCE WOMEN’S ENGAGEMENT TO PMTCT SERVICES: COUNSELLING
WOMEN WITH DOUBTS REGARDING ARV EFFICACY EARLY PROGRAM: ENHANCMENT OF SUPPORT
FOR WOMEN IN NEED; A CONTINUOUS CAMPAIGNS; AVAILABILITY OF ADEQUATE HUMAN
RESOURCES; REDUCTION OF LONG WAITING TIMES, AND INCREASED PRIVACY DURING RETURN
VISITS
Conclusions
Our study argues the clear
importance of motivating factors that outweigh barriers to PMTCT uptake and
adherence at five levels of the socio-ecological framework. The roll out of
Option B + as policy for pregnant women in Papua, which means inclusion of HIV
testing as a routine part of pregnancy screening, has improved identification
of HIV-positive women and their enrolment in the program. Further strengthening
of the PMTCT program is necessary to ensure continuous enrolment of new cases
while maintaining adherence of women in HIV care by addressing barriers or
potential inhibitors to long-term treatment. These
include availability of strategies to identify and counsel women with doubts
regarding ARV efficacy early in the program, establishment of support for women
in need, a continuous campaign to reduce stigma and discrimination at the
community level, availability of adequate human resources, reduction of long
waiting times, and increased privacy during return visits.


Comments
Post a Comment