Book: Social Determinants of Health; A Comparative Approach
Social Determinants of Health; A
Comparative Approach
REFERENCE
Davidson,
Alan, 2015, Social Determinants of Health, a Comparative Study, Oxford, Canada
MY
SUMMARY
As an Epidemiologist, I understand that my health is associated with
three main factorsà agent, host, and environment. If my immunity is weak (host), and
my children got flu from her childcare and then sneeze (agent:virus), then the
weather is winter (environment), make me susceptible to get Flu. However, if I
consider as an Social Epidemiologist, I should consider other factors, like my
wealth, education, my insurance, health care availability and accessibility, my
work that might increase or decrease my susceptibility to get flu or not.
Therefore, a term known as ‘SOCIAL DETERMINANTS OF HEALTH that provides
multiple layers of factors that might contribute to the complexity of health
condition, including Place, where we live and work, risk factors-behavior,
diet, stress, access to health care, social interaction-social support, social network,
biology-age, sex and gender, socio-economic status-education, income.
For
instance, in my research, some HIV-positive women’husband can survive after
being tested as HIV persons, while other were getting severe and then died. They
already have virus in their body (agent), therefore how they have good immunity
and healthy environment to keep survive. By understanding determinants of
health, I learn how social support and psychological support from their wife
and family are necessary. Their wife kept treating their husband, never shared
about their CD4 level, and got a reminder from their husband we should be
strong to raise their children. Although HIV virus has impacted on their
immunity and cause some opportunistic infections, like Tuberculosis, Pneumonia
and rash on their skin and they had very low CD4 (under 50), they finally can
survive and keep accessing ARV treatment. In addition, their husband starts to
reduce or even stop smoking, and eat much healthier food and avoid stay overnight.
They believe that unhealthy behaviors will threaten their immunity and make
them easy to fall sick because HIV is in their body (health belief model).
DIRECT QUOTATION
The conventional understanding of health
focus on some terms of susceptibility or our resilience, risk factors, triangle
of epidemiology (host, agents &
vector, and environment), population at risk, population attribute etc. Risk
factor analysis is useful = powerful way of looking at human health (p.4).
Population
health refers to the health of a population as measured by health status
indicators and as influenced by social, economic and physical environments,
personal health practices, individual capacity and coping skills, human
biology, early childhood development and health services. As an approach, population
health focuses on the interrelated conditions and factors that influence the
health of population over the life course, identifies systematic variations in
their patters of occurrence, and applies the resulting knowledge to develop and
implement policies and actions to improve the health and well-being of those
populations (emphasis added) (Public Health Agency of Canada, 2012) p.7
Determinants of population health:
1. Income and social status
2. Social support networks
3. Education and literacy
4. Employment and working conditions
5. Social environments
6. Physical environments
7. Personal health practices and coping skills
8. Healthy child development
9. Biology and genetic endowment
10. Health service
11. Gender
12. Culture (Public Health Agency of Canada, 2013) p. 8
Understanding health inequalities and health
inequities
if a child developed a condition that current medical technology
cannot diagnose and because of that no effective treatment could be applied and
the child died, that would be unfortunate but not unfair. If the child was not
diagnosed because her mother could not afford the hospital’s fees and, in
consequence of not receiving care that would have otherwise been available, she
died, that would be not only unfortunate, but also unjust. At the social level,
failing to respond to a harmful social circumstance that is within our
collective power to change is an injustice. Health inequalities arise from
conditions over which we have no control; health inequities or injustices,
arise from conditions which are amenable to collective action. P.9
Social Epidemiology is the branch of epidemiology that studies how social position and
context influence human health, on the other hand clinical epidemiology which
focus on rsk factors within a host-agent model. P. 43
Four main features characterize social epidemiology:
1. SE takes a population-level perspective
2. SE concerns itself with the social context of behavior
3. SE relies on multi-level analyses
4.
SE takes a developmental,
life-course perspective.
Psychosocial Theories
The feelings of stress that arise regarding an individual’s position
ultimately drive his or her health status. At first glance, this appears to be
quite a load to be carried by stress. But keep in mind that stress
significantly impairs our capacity to cope with challenges. Moreover, chronic
stress has been linked to smoking, excess alcohol consumption, over eating,
depression, and breakdown of social relations. People under stress have a
heightened sensitivity to pain and are susceptible to debilitating chronic pain
syndromes. And there is evidence that stress can affect basic metabolic
pathways, contributing to diabetes and impaired immune function. Chronic stress
is also associated with coronary heart disease. (p.1)
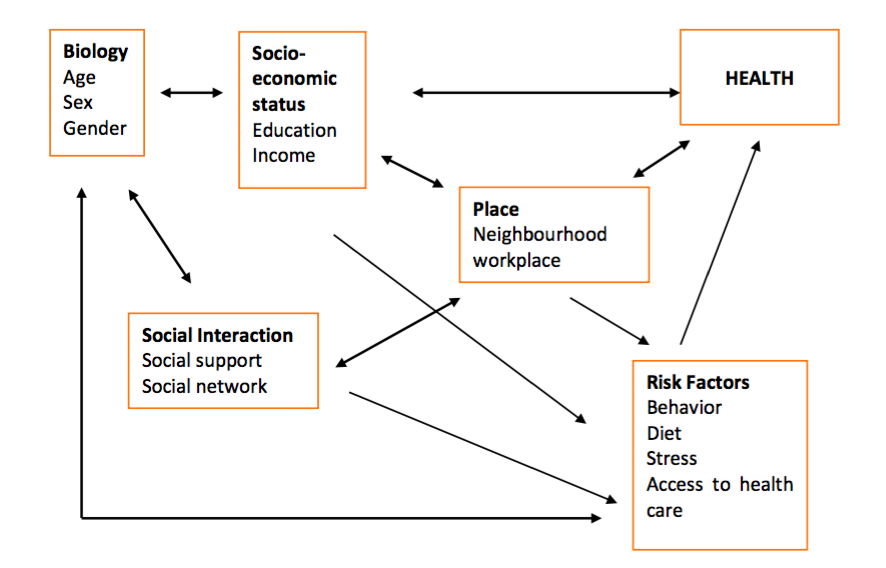
Place, where we live and work, risk factors-behavior,
diet, stress, access to health care, social interaction-social support, social network,
biology-age, sex and gender, socio-economic status-education, income
Figure 2.8. Conceptual Model
of Determinants of Health (p.enam puluh dua)
Recall there are three: materialist, neo-materialist, and
psychosocial. The key difference is that materialist hypotheses construe the
main driver of health differences to be individual resources or capacities,
whereas psychosocial hypotheses construe differences in health to arise from
differences in social status or rank.
The Psychosocial Model
Figure 3.
Psychosocial Income Inequality Pathways to Poor Health (page 93)
an alternative
to materialist thinking is psychosocial theorizing. The pathway from society to
our biology is our perception, particularly our perceptions of our status and
personal security. A sense of lack of respect or fearfulness can prime our
stress response leading to chronic strain and elevated levels of cortisol which
in turn damage our emotional, mental and physical health. (p.92)
MATERIALIST THEORY
It links
individual level considerations such as income available to a person or a
household to health outcomes through a family of hypotheses (p.92)
NEO-MATERIALIST
ANALYSIS is inherently multi-level because social structures, processes, and
public goods (all collectice features) may provide key health-relevant
resources to individuals. Thus theory in this gendre consider jointly
collective-and individual level resource relevant features.
SOCIAL PATTERNING OF BEHAVIOUR
it is a serious
mistake to construe health-relevant behavior as “individual” in the sense that
it is chosen, albeit shaped by external factor (237)
The Health Belief Model
According to
Rosenstock (1974), the model relies on four key variables:
1.
Self-perceived personal risk
2.
Self-perceived severity of the
outcomes associated with unhealthy behavior
3.
Self-perceived barriers to and
costs of behavioral change; and
4.
Self-perceived benefits of
making the behavioral change
Health belief Model
Health behavior as socially Patterned
·
Rationale behavior and
incentives
·
Rationale behavior and
information
·
Rationale behavior and our
brain
·
Rationale behavior and
sociology



Comments
Post a Comment